Macular Degeneration
- Home
- Macular Degeneration
What is it?
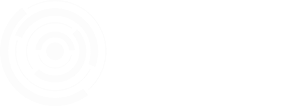
Age Related Macular Degeneration (AMD) causes loss of central vision. It is caused by a problem in the retina, which is the light sensitive layer at the back of the eye, much like the film is the light sensitive layer at the back of a camera.
Image: Eye and macular anatomy
The macula is the central part of the retina that is responsible for the detailed, central vision.
Image: Macular resolution

This image demonstrates normal vision. The macula, in the centre of the retina, is able to see greater detail than the periphery. The outer edge of our normal vision is blurred.
AMD results from damage to the macula. The rest of the retina is not affected. The only part of the vision that is affected is the very central area, which is often just an indistinct blob. The size and extent of the vision loss depends on the extent of the macular damage.
Image: AMD simulation

This image represents the vision in AMD. There is normal loss of detail from the centre to the periphery, but in this case, there is also loss of central vision.
Broadly speaking there are two forms of AMD. Dry and Wet.
Dry AMD is due to wear and tear. Think of a carpet, that becomes increasingly worn until only the cords remain.
There are varying degrees of AMD. In the early stages the macula may still be functioning well, and the vision remains good. Slit lamp examination will identify specific changes, which include pigment changes in the retina as well as pale spots, called drusen. Drusen and pigment change are early visible changes that indicate a deterioration in the health of the retina.
In more advanced disease the retina becomes completely worn out and the underlying layers become exposed through these defects. This is known as geographic atrophy, which refers to the shape of these defects (geographic) and the fact that the retina has wasted away (atrophy).
On the whole dry AMD is less severe and progresses more slowly than wet AMD. However, geographic atrophy can be devastating if the defect is large and central, and the effect on the vision can be as significant as wet AMD.
If dry AMD is like a worn carpet, then wet AMD is like a burst waterpipe under the carpet. The process that characterises wet AMD is called choroidal neovascularization. This term means, new blood vessels that come from the choroid, which is a layer under the retina.
In our carpet analogy, if the retina is the carpet then the choroid is the underfelt.
New vessels grow from the choroid because they are stimulated to do so. The stimulus is a substance that is produced by the body, called Vascular Endothelial Growth Factor, often referred to simply as VEGF. In fact, there are likely to be many factors that lead to choroidal neovascularization and this is an area of intensive research, but for the purpose of this explanation it is useful to focus on VEGF. The reason will become clear when we discuss treatment.
The new blood vessels that grow from the choroid are not normal, healthy vessels. They are not robust, and they tend to leak. They are also fragile and tend to rupture and bleed. All this leaking fluid and blood ends up in the retina. The retina is a very complicated and delicate structure, and this type of insult can be devastating. The elegant architecture of the retina, which is so important for its function, is disrupted which results in vision loss. As we noted earlier, this disruption tends to occur in the centre of the macula.
Do I have it?
AMD is by definition, age related. If you are under the age of 50 years, it is very unlikely that you have AMD. However, there are other conditions that may affect central vision in younger people.
The risk of developing AMD increases with increasing age, particularly if there is a family history, but other conditions may also affect the vision in this age group and the diagnosis will require confirmation by an ophthalmologist.
Early AMD is often asymptomatic and discovered as a coincidental finding during a routine examination. There may be some difficulty with night vision, and this will deteriorate further as the disease progresses.
In time the central vision may become blurred and colours may appear less bright. Visual distortion may occur, and central vision becomes increasingly limited.
In advanced AMD it becomes difficult to recognise faces and vision deteriorates further.
Distortion becomes more pronounced and may be associated with choroidal neovascularization.
Dry AMD
There is no proven effective treatment for dry AMD. However, this is not to say that nothing should be done. There is a risk of developing advanced dry AMD or wet AMD and it is important to know about the following risk factors.
- Diet high in saturated fats
- Alcohol consumption
- Overweight
- Smoking
- Family history of AMD
- Over the age of 50
- Hypertension (high blood pressure)
- Caucasians have an increased risk of wet AMD
Patients with dry AMD who have numerous drusen or large drusen are at increased risk of developing wet AMD. However, this group of patients can reduce their risk by taking a supplement in the proportions outlined in the AREDS2 study. These are as follows.
- Vitamin C (500mg)
- Vitamin E (400mg)
- Lutein (10mg)
- Zeaxanthin (2mg)
- Zinc (80mg)
- Copper (2mg)
There are several manufacturers that produce this formulation. It is also advised to eat a diet rich in dark green leafy vegetables and yellow fruit and vegetables.
Wet AMD
There is very effective treatment for wet AMD.
You may recall that VEGF is, at least in part, responsible for the process of neovascularization that leads to wet AMD.
Only free VEGF can stimulate neovascularization and research has led to the production of a drug that binds to VEGF, thereby rendering it ineffective. These drugs are known as anti-VEGF drugs.
Treatment is by means of an injection under topical anaesthesia. Less than half a drop of anti-VEGF is injected, using a very fine needle, through the sclera (white part of the eye), into the vitreous (gel in the eye). The injection process takes about 1 second and is very well tolerated, in spite of the initial apprehension that most patients experience. Anti-VEGF will not remain in the vitreous indefinitely. Eventually the levels of VEGF increase and the level of anti-VEGF drops, and the abnormal vessels start leaking again. The injection needs to be repeated intermittently to keep the VEGF levels under control.
Control means that there is no active fluid in the retina. We use an instrument called an Optical Coherence Tonometer (OCT) to look at the retina in fine detail at every visit.
Image: OCT

The OCT will identify fluid in the retina. When the fluid is controlled the vision remains stable. Initially injections are given every 4 weeks. However, not all patients will reactivate after 4 weeks. Some may only reactivate after 12 weeks, or even longer.
Every patient appears to have a reactivation interval that is likely to be related to their genetic makeup and risk profile. It may change but tends to be quite stable.
We determine this interval by gradually increasing the time between injections and checking for reactivation (when fluid reappears in the retina). The aim is to safely increase the interval as much as possible.